
Brits have been urged by experts to beware of the growing cases of an illness which can be mistaken for the common flu or cold.
In recent weeks, China has seen a sharp increase in cases of the illness, leading people to fear another worldwide outbreak.
HMPV, or human metapneumovirus, is most common among children, with countries such as India, Kazakhstan and Malaysia also seeing an increase in cases.
If some patients aren’t careful, it can lead to other health complications, such as respiratory issues.

The illness is starting to spread quicker (Getty Stock Photo)
What is HMPV?
The virus first surfaced in 2001, and like the flu, it can be spread through sneezing, coughing, or contact with contaminated surfaces.
Similar to respiratory syncytial virus (RSV), it is a seasonal virus that thrives in colder weather and mostly affects children under the age of five.
But before you start comparing it to Covid-19, it should be noted that it’s a regular seasonal illness that has come and gone across the world for decades, so there is more resistance among the general population, The Independent says.
What are the symptoms of HMPV?
There are a number of symptoms to look out for, according to Public Health Scotland, such as:
- Coughing
- A fever (high temperature)
- Nasal congestion (runny nose)
- Fatigue
These symptoms can take anywhere between three and six days to clear, and while there are no vaccines or specific treatments for the sickness, it should be gone within a week.

The condition is similar to having the flu (Getty Stock Photo)
Are cases of HMPV increasing in the UK?
Unfortunately, the answer here is yes.
The latest data from the UK Health & Security Agency (UKHSA) reveals that cases of HMPV are ‘increasing slightly’, with 4.5 percent of lab tests being positive between 23 and 29 December.
READ MORE
COMMON MISTAKE THAT COULD LEAVE WATER BOTTLE DIRTIER THAN TOILET SEAT
DOCTOR EXPLAINS EASILY MISSED SYMPTOM OF CANCER THAT WAS ‘VERY RARE’ BUT NOW ON THE RISE
Compared to the flu, which has 29.5 percent of lab tests positive during the same period, it looks OK, but compared to Covid, it is higher as the latter stood at 2.5 percent.
However, as there is more of a global resistance to HMPV, it is highly unlikely that it will reach anywhere near the scale of the coronavirus pandemic.
What are experts saying?
Professor John Tregoning, who is an expert in vaccine immunology at Imperial College London, has compared the illness to RSV, explaining to The Daily Mail: “It is part of the cocktail of winter viruses that we are exposed to and, like other viruses, it will transmit in coughs, sneezes and in droplets.”
He added that staying in ‘well-ventilated spaces’, and simple things such as covering your mouth when you cough and washing your hands often can help to stop spread the illness.
He also noted that antibiotics won’t have an effect as it is a virus, and the main treatment is to manage symptoms.

Those in higher risk categories should visit the GP if they show any of the main symptoms (Getty Stock Photo)
Professor Jaya Dantas at Curtin University in Australia explained that we have to ‘wear a mask in public’ and stay away from others to protect the vulnerable.
“In young children, the elderly and those who are immune compromised, HMPV can lead to severe cases and can move to the lower respiratory tract and may lead to pneumonia,” the expert explained.
Another professor, Jonathan Ball, who works at Liverpool School of Tropical Medicine, highlighted: “HPMV has been known about since 2001, and has been circulating in humans for at least 50 years – probably a lot longer. Unfortunately, it is associated with pneumonia, particularly in young children, but this is thankfully rare.”
Meanwhile, Professor Paul Hunter from the University of East Anglia, added: “Almost every child will have at least one infection with HMPV by their fifth birthday and we can expect to go on to to have multiple reinfections throughout life.
“It is one of the leading viral causes of respiratory infections in children under five-year-olds.”
How can you test for HMPV?
HMPV symptoms will fade within a week for those that are healthy and going through mild conditions, so a trip to the GP is usually not necessary.
But those in higher risk categories, such as those with respiratory problems, a weak immune system or old age, may want to visit the GP to be safe.
If you’re experiencing intense symptoms, it is advised that you visit the GP, where they will provide a test is necessary.
Some of these severe symptoms are bronchitis, bronchiolitis and pneumonia, as well as a shortness of breath or wheezing.
Brits are being warned after cases of a brutal illness are hitting the shores of the UK earlier and in bigger numbers than usual for autumn.
We’re of course talking about the highly infectious norovirus, which, if you’ve not had, you definitely do not want.
Usually a condition that is more common in the colder winter months, norovirus – or the ‘winter vomiting bug’ – is making an early break for it, despite autumn being incredibly mild so far.
The most recent NHS data shows that infections are up 29 percent between 23 September and 6 October, a level that is double the usual outbreak level for this time of year.
Here’s everything you need to know to prepare and protect yourself from norovirus.

We’ve all been there (Getty Stock Images)
What are symptoms of norovirus?
Norovirus is not just a standard tummy bug. Instead, it can be incredibly unpleasant, and leave you lacking the energy to do anything at all.
The three main symptoms of the stomach bug is feeling sick, having diarrhoea, and then actually being sick.
Other symptoms include having a high temperature, headaches, and aches throughout your arms and legs.
You can get these symptoms suddenly, appearing usually between one and two days after exposure.
How do I treat norovirus?
The main thing to do when suffering from norovirus is to keep your fluid intake up, as you’re be losing a lot of it via two of the three main symptoms. Small sips might be the best approach to stop a sensitive stomach from reacting.
Over-the-counter painkillers can alleviate discomfort, and you should avoid spicy or fatty foods, eating plain meals when you are able to.
To avoid getting norovirus in the first place, you should limit your physical contact with surfaces or objects that could have the virus on them. If you do touch them, such as the handle of a door, don’t touch your mouth and wash your hands after doing so.
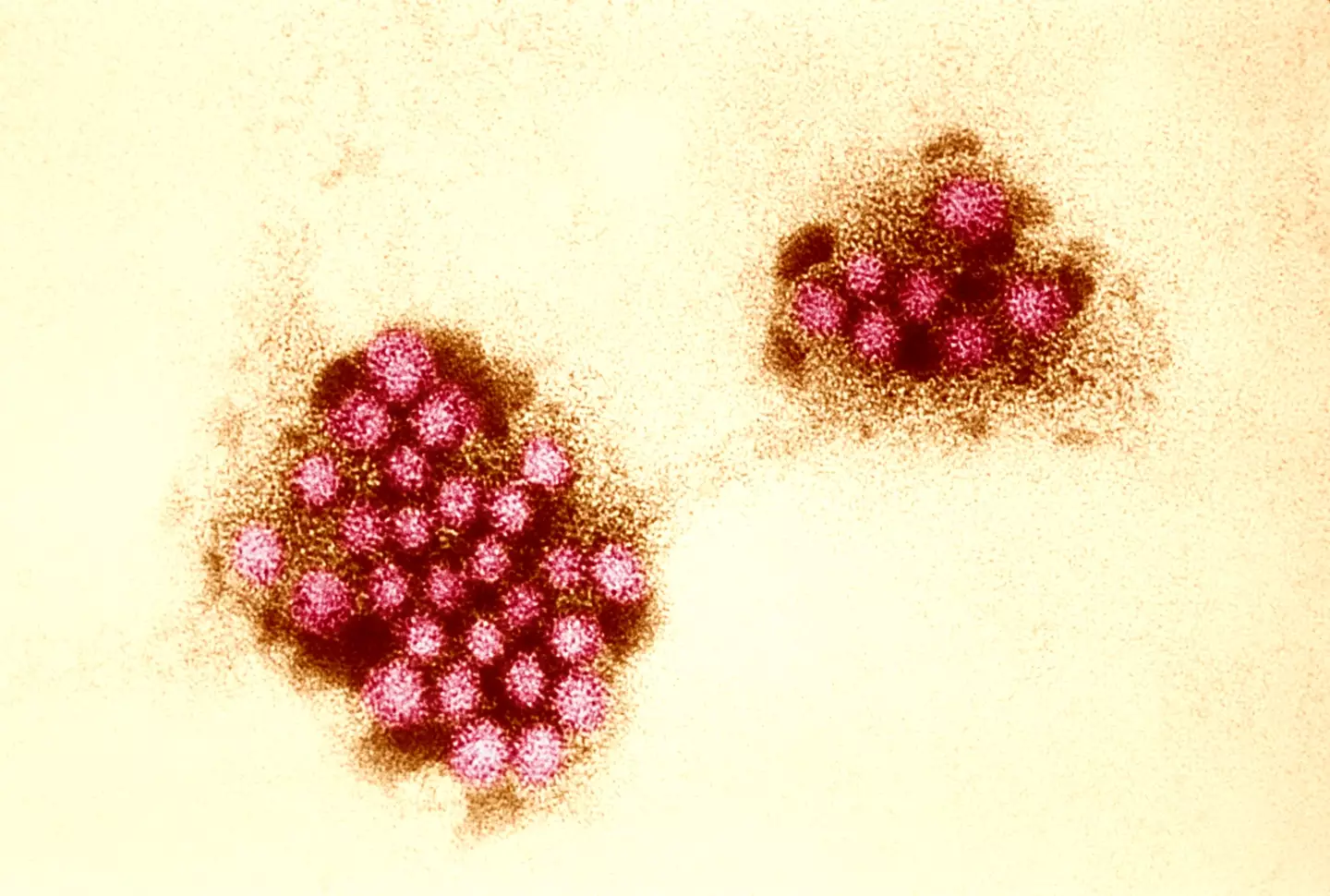
Norovirus close up under a microscope (BSIP/UIG Via Getty Images)
Norovirus ’48-hour’ warning
People who experience symptoms of norovirus have also been told to stay away from workplaces or schools for a 48-hour period after they start to impact you.
You are also advised to not visit doctor surgeries, hospitals, or care homes, so as not to spread the illness through people who might be more prone to infection.
Hospital infections are currently 22 percent higher than standard, official data says.
Amy Douglas, an epidemiologist at the UK Health Security Agency (UKHSA), said: “Norovirus levels have remained higher than expected recently and cases are likely to increase.
“To help reduce the spread of the infection, if you have diarrhoea and vomiting, take steps to avoid passing the infection on.
“Do not return to work, school or nursery until 48 hours after your symptoms have stopped, and don’t prepare food for others in that time either. If you are unwell, avoid visiting people in hospitals and care homes to prevent passing on the infection in these settings.”

One of the best ways to stop infection is to wash your hands (Getty Stock Images)
Does hand sanitiser work against norovirus?
Douglas has warned Brits that you cannot stop norovirus from using hand sanitiser alone.
“Alcohol gels do not kill norovirus so don’t rely on these alone,” she explained, meaning that most hand gels would not be enough to stop it from getting you, should you happen to come into contact with it.
Instead, properly washing your hands is the way to go, like how we were told to during the Covid pandemic.
She said: “Washing your hands with soap and warm water and using bleach-based products to clean surfaces will also help stop infections from spreading.”

There is one cancer symptom that UK residents should keep their eye out for this summer, according to a doctor.
It’s something that all of us will go through in the coming months, and it’s worth keeping tabs on, as though many may think it’s normal, it could indicate something serious for your health and well-being.
As the summer months have arrived (apparently), the temperature is set to rise and be higher than it has been recently (again, apparently), as the UK enters a period some warmer and more pleasant weather.
Though some of us may be sat staring out of the window and witnessing a downpour in the middle of June, there is the comfort of knowing that we’re not even two weeks into summer.
It couldn’t get any worse, could it? I guess time will tell.

Warmer weather could mean a number of things. (Getty Stock Photo)
When the temperature gets up there, our body responds by producing sweat, which cools our body temperature down, keeping it regulated and stopping us from getting heat stroke or shutting down altogether.
During the day, the heat may leave our soaks more soaked than normal, but it turns out that it may not be as normal of an occurrence at night.
You may find yourself dismissing the severity of sweating in your sleep in this weather, because it is summer after all.
However, a doctor has warned that night sweats could easily signal serious health issues, with one of these being cancer.
Dr Suhail Hussain is a personal physician and private home visiting GP, and has urged Brits to look out for sweating at night – especially if it is common.
“Sweating at night is a common phenomenon and one that is far more likely to happen on hot sticky nights such as we’re experiencing now,” he explained as per The Daily Express.
“However, the occurrence of such symptoms should not merely be dismissed as, ‘Oh well it’s just hot outside’.
He revealed: “Night sweats can be a sign of something more serious, for example, serious infections, the menopause and even cancer.”
There is a difference between regular night sweats and potentially cancerous ones though – and it’s important to note the contrast from one to the other.

There are a number of signs that can indicate if you’re having cancerous cold sweats. (Getty Stock Photo)
Dr Hussain said: “Sweats associated with cancer are normally drenching – literally. You can wake up with your pyjamas and bed sheets wringing wet with sweat.”
As well as this, the medical expert highlighted other glaring signs that, if seen, should be brought up with a doctor:
- Persistent and sweats that aren’t remitting – regular night sweats will usually be intermittent.
- Fatigue or a lack of energy in day-to-day life.
- Unexplained bruises on your body
- Inexplicable pain
- Lymph node enlargement
- Sweating in the day that isn’t related to being too hot at night.
The most common cause of cancerous night sweats are leukaemia and lymphoma – which are cancers related to the blood and lymph mode systems.
This is why you may see enlarged glands and find yourself easy to bruise.
He further explains that rare forms of cancer can also cause sweating, with this group known as ‘carcinoids’.
By affecting hormonal function through the neuroendocrine system, it can result in excess sweating.
Dr Hussain said: “Other concomitant symptoms could include flushing of the skin, alterations in pulse and blood pressure and muscle and joint aches.
“The bottom line is that if you feel like sweaty Betty or perspiring Pete and it’s going on a bit too long, then head over to your GP and get checked out.”

A doctor who was diagnosed with leukaemia has revealed a surprising symptom she almost ignored.
Ellissa Baskind, 46, has spent much of her working life carrying out operations as a consultant gynaecologist in Leeds.
Over the years, she developed progressively worse back pain, something she put down to the nature of constantly be bent over in her job.
It was at her work Christmas party however, when Ellissa thought something was up after she was left unable to dance due to the pain.

Dr Ellissa Baskind says ‘don’t ignore your symptoms’ (Kennedy News and Media)
Naturally being in the medical field, she went and got an x-ray which came back clear. However, her blood results came back with abnormalities and the mum-of-two was given a shock leukaemia diagnosis.
Ellissa said: “At the time [I was diagnosed] I was doing a lot of operations and you do get yourself into a lot of awkward positions. It’s just the nature of the job.
“It’s not uncommon in my line of work to have back pain. I was getting pain in my shoulder blades which was keeping me up at night.
“Even as a doctor, you don’t think of the worst things. I genuinely thought it was related to my work. I never once thought it was something sinister.

Ellissa was diagnosed with acute myeloid leukaemia (Kennedy News and Media)
“I wasn’t sure I would make it to the Christmas party because this pain was bothering me so much. It was at the forefront of my mind. The pain stopped me from dancing and being able to enjoy myself fully.”
Ellissa was diagnosed with acute myeloid leukaemia – a cancer of the myeloid line of blood cells, characterised by the rapid growth of abnormal cells.
Having to undergo two rounds of chemotherapy, Ellissa then discovered a lump in her breast and was diagnosed with myeloid sarcoma 18 months later.
Ellissa said: “Looking at the literature, there is no cure for myeloid sarcoma. I believed it was palliative. That night I was looking into hospice care and thought it was the end of the road.
“The doctors asked me how much fight I had left in me and I said I’m only interested in a cure. They said there is a chance of a cure but it’s very remote and you would need another stem cell transplant.”

Ellissa said she ‘could have so easily just gone on with my life and missed it’ (Kennedy News and Media)
After undergoing successful stem cell transplant in 2022, she did two more rounds of chemotherapy in June.
Ellissa added: “I’m now in the best health and have hit five years now which is a real milestone. I’m very fortunate.
“The best advice I have to people going through cancer treatment is to take each day at a time. I feel so lucky to be alive. And it’s changed the way I approach patients having been one myself.
“I look back and I felt very well other than that back pain. I could have so easily just gone on with my life and missed it. “Please listen to your body and don’t ignore your symptoms; keep pursuing answers and persevere until you know what is going on.”
If you’ve been affected by any of these issues and want to speak to someone in confidence, contact Macmillan’s Cancer Support Line on 0808 808 00 00, 8am–8pm seven days a week.

A dentist has issued a warning to those suffering from a health issue that often worsens in the winter months.
When it comes to signs of illness, most of us know to look out for any unusual changes within our bodies, such as lumps or ongoing pain.
But there are certain signs that can be easily dismissed as something totally different.

A dentist has issued a warning over a common winter complaint (Getty Stock Photo)
In case you didn’t know, a number of health conditions can also be linked to oral health.
And now, an oral surgeon has explained one sign to look out for which could indicate something more serious.
Dr Andrej Bozic is an oral surgeon at Dentum. He explained that while mouth ulcers can be common in winter, it’s worth keeping an eye on them to see how long they last.
Mouth ulcers can be caused by biting the inside of your cheeks, having poorly fitted dentures or braces, from cuts or burns, allergies, damage to your gums, and stress.
However, they can also be caused by other factors such as hormonal changes, genetics, vitamin deficiencies, and certain medications.
While it can be normal to suffer with mouth ulcers every now and then, they should really heal up within a couple of weeks.

Mouth ulcers can be pretty painful (Getty Stock Photo)
“Most mouth ulcers heal within 10 to 14 days,” Dr Bozic told the Mirror.
“If a sore lingers beyond that, it could indicate something more serious, such as oral cancer, an autoimmune disease, or a chronic infection.
“Dehydration and a higher risk of infections during colder months can aggravate mouth ulcers. But any sore that persists shouldn’t be dismissed as seasonal – it’s crucial to have it checked.”
It’s concerning if the ulcer does not heal after three weeks, or if there’s red or white patches inside the mouth and any unexplained pain.
Difficulty chewing, swallowing or speaking, or any lumps or swelling in the neck or jaw should also be investigated by a healthcare professional.
The NHS also explains that you should visit the doctor if the ulcer:
- lasts longer than three weeks
- is different to other mouth ulcers you’ve had before, for example if it’s bigger or in a different location, such as the throat
- bleeds or becomes more painful and red

A mouth ulcer should clear up within a couple of weeks (Getty Stock Photo)
“A non-healing ulcer is one of the early warning signs of oral cancer,” Dr Bozic added.
“Patients often dismiss these as minor injuries, but an ulcer that lasts more than three weeks should be taken seriously. It’s crucial to look for other symptoms like red or white patches or lumps in the mouth.”



